
What Causes Under-the-Skin Pimples and How to Treat Them?
Under-the-skin pimples, also known as subcutaneous acne, are one of the most frustrating skin issues many people experience. Unlike typical acne that appears on the
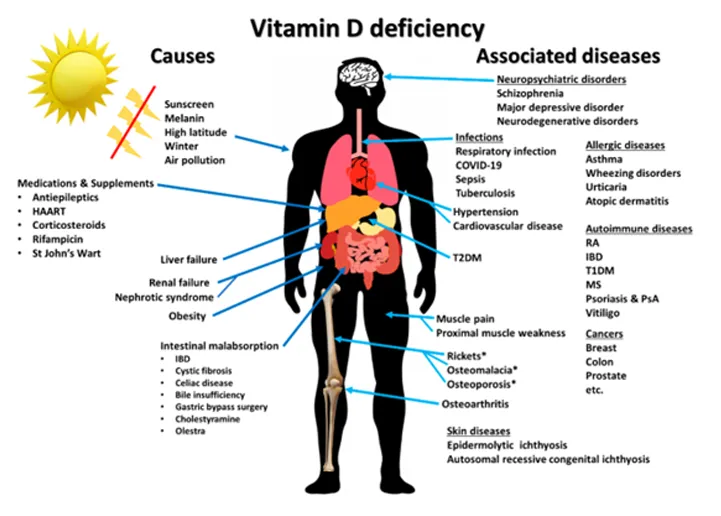
Vitamin D is classically known to regulate calcium and phosphate metabolism. It not only plays an essential role in maintaining healthy mineralized skeleton, but also is an immunomodulatory hormone]. Both the vitamin D receptor (VDR) and metabolizing enzymes are expressed by various types of immune cells including lymphocytes, monocytes, macrophages, and dendritic cells. Experimental studies have shown that vitamin D has significant biologic activities on the innate and adaptive immune systems. Animal studies have demonstrated that administration of vitamin D or its metabolites leads to changes in the occurrence and progression of various immune-related diseases This supports the clinical and epidemiological data that link vitamin D with the incidence and severity of many disorders such as psoriasis, multiple sclerosis, rheumatoid arthritis, type 1 diabetes, and infectious diseases The purpose of the present review is to provide a high-level summary of the biologic effects of vitamin D on the immune system and the relationship between vitamin D and several types of immune-related diseases and conditions. This review also aims to give some perspective about the heterogeneity of evidence on the impact of vitamin D on prevention and treatment of immune-related diseases and to introduce the concept individual responsiveness to vitamin D as a potential explanation for such heterogeneity.
Historical evidence that links vitamin D with innate immunity came from the reports in the mid-1800s and early 1900s prior to the antibiotic era that vitamin D3-rich cod liver oil and sunlight exposure were used for treatment of tuberculosis (TB) [16]. Later, subsequent studies have identified the explanation for the therapeutic effects of cod liver oil and sunlight. In the presence of infection, activated macrophages and monocytes, induced by toll-like receptor signaling and exposure to inflammatory cytokines such as interferon-Ƴ (IFN-Ƴ), strongly express CYP27B1 which converts 25(OH)D into 1,25(OH)2D [17]. Then, 1,25(OH)2D enhances antimicrobial activities of macrophages and monocytes in an autocrine fashion via VDR-RXR signaling, which, in turn, stimulates the production of endogenous antimicrobial cathelicidin LL-37 . Cathelicidin acts against invading bacteria and fungi by destabilizing microbial membranes . It also exhibits direct antiviral activities against many respiratory viruses by disrupting viral envelopes and altering viability of host target cells . This process is especially robust in granulomatous inflammation such as TB, fungal infections, sarcoidosis, and some lymphomas. The macrophage production of 1,25(OH)2D not only is for the purpose of upregulating the production of cathelicidin LL-37 but also produces it so that it can exit the cell and influence nearby lymphocyte function). However, an unintended consequence of this paracrine function is that the macrophages produce an excess amount of 1,25(OH)2D that enters the circulation and an unregulated fashion stimulates intestinal calcium absorption and bone calcium mobilization resulting in hypercalciuria and hypercalcemia . This is more likely to occur when circulating levels of 25(OH)D are above 30 ng/mL (75 nmol/L) , which is the explanation for why patients with granulomatous disorders including sarcoidosis develop hypercalcemia during the summer.
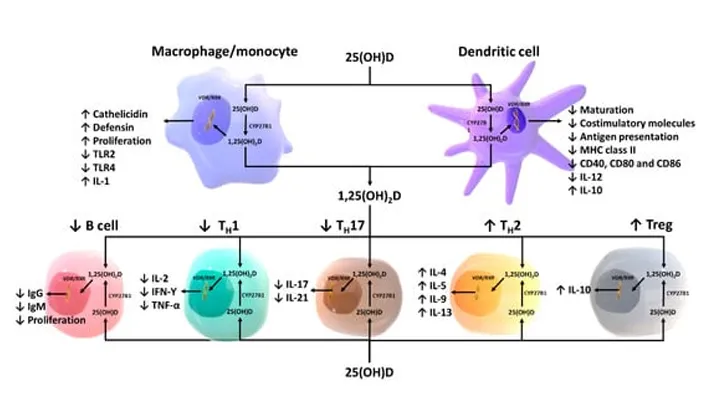
Figure 2. Schematic representation of paracrine and intracrine function of vitamin D and its metabolites and actions of 1,25-dihydroxyvitamin D on the innate and adaptive immune systems. Abbreviation: 1,25(OH)2D: 1,25-dihydroxyvitamin D; 25(OH)D: 25-hydroxyvitamin D, IFN-Ƴ: interferon- Ƴ; IL: interleukin; MHC: membrane histocompatibility complex, TH1: T helper 1; TH2: T helper 2; TH17: T helper 17; Treg: regulatory T cell, TNF-α: Tumor necrosis factor- α; TLR2: toll-like receptor 2; TLR4: toll-like receptor 4. Reproduced with permission from Holick MF, copyright 2020.
1,25(OH)2D modulates the differentiation and functions of antigen-presenting cells by inducing them to become more immature and tolerogenic, characterized by a decrease in the expression of major histocompatibility complex (MHC) class II and co-stimulatory molecules on the cell surface [). This results in a decrease in antigen presentation and production of interleukin-12 (IL-12), and an increase in production of IL-10, a tolerogenic cytokine [,]. 1,25(OH)2D is also shown to suppress the expression of toll-like receptors on the monocytes and inhibit the production of some inflammatory cytokines such as IL-2, IL-6, and IL-17 []. In addition, experimental studies have suggested that differentiation and function of natural killer (NK) cells can be modulated by 1,25(OH)2D treatment. However, whether 1,25(OH)2D induces or inhibits NK cell function is still unclear as data regarding the influence of 1,25(OH)2D on NK cells are inconsistent
A number of experimental studies have shown that vitamin D and its metabolites modulate endothelial function and vascular permeability via multiple genomic and extra-genomic pathways. For instance, Gibson et al. [] demonstrated in the primary dermal human microvascular endothelial cell model that vitamin D3, 25(OH)D3 and 1,25(OH)2D3 non-genomically stabilized vascular endothelium, and that vitamin D3, normally circulating at about 100 times higher level than 1,25(OH)2D3, was at least 10 times more potent than 1,25(OH)2D3 and more than thousand times more potent than 25(OH)D3 in stabilizing the endothelium. Studies have also shown that 1,25(OH)2D3 is a transcriptional regulator of endothelial nitric oxide synthase (eNOS), causing up-regulation of eNOS gene expression and therefore increased endothelial production of nitric oxide. Interestingly, Molinari et al. [] observed that the effect of 1,25(OH)2D3 on endothelial nitric oxide production occurred most robustly within one minute after administrating the compound, implying that the action of 1,25(OH)2D3 was non-genomic. Activation of VDR by 1,25(OH)2D at the endothelial cell membrane is shown to increase eNOS activity via intracellular second messenger pathways including adenylyl cyclase/cyclic adenosine monophosphate (AC/cAMP) and inositol trisphosphate/diacylglycerol (IP3/DAG) pathways, which result in increased intracellular calcium concentration. Activation of VDR also activates eNOS via the phosphoinositide 3-kinase/protein kinase b (PI3K/Akt) pathway that triggers phosphorylation of serine-1779 on eNOS []. Furthermore, Cuenca et al. [] showed in a uremic rat model using the immunofluorescence technique that 1,25(OH)2D2 promoted vascular endothelial-cadherin-based cell–cell junctions and inhibited F-actin stress fiber organization, thereby preventing the formation of endothelial intracellular gaps and attenuating endothelial damage in the presence of chronic kidney disease. Taken together, it is evident that vitamin D and its metabolites exert pleiotropic effects on the vascular endothelium that are protective against vascular dysfunction and tissue injury as a result of local and systemic inflammation.
Multiple studies have shown that vitamin D plays a role in maintaining gut integrity and intestinal homeostasis between host and gut microbiota. Vitamin D signaling is shown to increase the viability of intestinal epithelial cells and and alleviate intestinal epithelial damages from bacterial lipopolysaccharide It promotes mucosal barrier function by enhancing the expression of intracellular pathogen recognition proteins and epithelial membrane junction proteins [45,46]. Moreover, 1,25(OH)2D induces the production and secretion of antimicrobial peptides by the intestinal epithelial cells, Paneth cells, and intraepithelial lymphocytes These result in limitation of gut bacterial translocation into the interstitium and maintenance of intestinal homeostasis, which are believed to involve in the pathogenesis of multiple autoinflammatory and metabolic disorders
Vitamin D plays an essential undisputed role in the maintenance of calcium, phosphate, and bone metabolism. There is compelling evidence that immune cells convert 25(OH)D to 1,25(OH)2D in an unregulated manner and are dependent on the circulating levels of 25(OH)D to be at least 30 ng/mL (75 nmol/L) Once a 1,25(OH)2D is produced, it acts in an autocrine and paracrine fashion to modulate the innate and adaptive immune systems. There is also some evidence that vitamin D itself may modulate immune function in a non-genomic manner by stabilizing endothelial membranes Most of the evidence, to date, suggests that maintenance of a healthy vitamin D status is important for modulating the body’s immune function. Low serum levels of 25(OH)D are associated with multiple immune-related diseases including autoimmune disorders and infectious diseases. There is less convincing evidence that vitamin D is an effective treatment strategy for autoimmune diseases and infectious diseases with a few exceptions documented in this review. Whether vitamin D therapy is effective as an adjunctive immunomodulatory agent for treatment of most diseases it is still controversial based on heterogeneous findings from the clinical trials.
National and international programs should be instituted to educate the public about the health benefits of vitamin D and policies to fortify commonly consumed foods with vitamin D to reduce the risk of vitamin D deficiency during pregnancy, childhood, and in young and middle-aged adults when autoimmune disorders are most prevalent. In addition, improvement in vitamin D status from birth until death may help reduce the risk of infectious diseases such as influenza and COVID-19 that can have devastating consequences especially for the elderly. However, more investigation is needed to determine who would most benefit from vitamin D, and how much vitamin D is required for its maximum health benefit based on their individual vitamin D responsive profile. It is also unknown whether giving 1,25(OH)2D3 or one of its analogs is a reasonable approach for treating autoimmune disorders and infectious diseases. Blood levels of 1,25(OH)2D3 are tightly controlled and for good reason, i.e., any significant increase in circulating levels of 1,25(OH)2D will result in an increase in intestinal calcium absorption and, when uncontrolled, this causes hypercalciuria and ultimately hypercalcemia. It is more likely that the endogenous production of 1,25(OH)2D in the immune cells including monocytes and macrophages is what is required for vitamin D to have its immunomodulatory functions.
Although most of the biologic effects of vitamin D have been related to its active metabolite there continues to be intriguing evidence that vitamin D itself may have its own biologic actions independent of its metabolism. Our hunter gatherer forefathers likely maintained serum vitamin D levels in the range of 10–50 ng/mL (25–125 nmol/L). This is supported by the observation that Maasai herders and Hadza tribesmen maintained serum 25(OH)D in the range of 40–60 ng/mL (100–150 nmol/L) To maintain these blood levels, a person would require ingesting approximately 4000–6000 IUs daily. This would therefore maintain circulating levels of vitamin D in the range of 20–40 ng/mL (50–100 nmol/L). The observation that in vitro vitamin D3 was much more effective than either 25(OH)D3 or 1,25(OH)2D3 in stabilizing endothelial membranes thereby reducing inflammation may help explain the interesting clinical observations that extremely high doses of vitamin D have been effective in treating or at least reducing symptoms of some autoimmune disorders including psoriasis, vitiligo, and multiple sclerosis. The observation that children with congenital autosomal recessive ichthyosis and epidermolytic ichthyosis had a dramatic improvement in their skin disease when treated with 60,000 IUs of vitamin D once a day for 10 days adds strength to the argument that vitamin D itself may have its own important role in the maintenance of good health There are still open questions that need to be further investigated in order to take full advantage of the effect of vitamin D on the immune system for clinical practice. The bottom line is that there is no downside to increasing our intake of vitamin D to maintain serum 25(OH)D at at least 30 ng/mL (75 nmol/L), and preferably at 40–60 ng/mL (100–150 nmol/L) to achieve optimal overall health benefits of vitamin D.

Under-the-skin pimples, also known as subcutaneous acne, are one of the most frustrating skin issues many people experience. Unlike typical acne that appears on the

Hair loss is a common issue faced by many individuals, affecting both men and women across different age groups. It can be caused by a

There isn’t one single food proven to prevent Alzheimer’s, but research suggests that a dietary pattern like the MIND diet can be beneficial for brain

Insomnia is a sleep disorder where you have trouble falling asleep, staying asleep, or both. There are actually no real advantages to insomnia. It disrupts